Nasal Septal Hole
Holes in nasal septum that divides the nasal cavity is called as nasal septum perforation. The hole can cause a direct communication between the two normally-separate sides of the nose and it can cause deterioration of physiological nasal air flow.
Nasal septal perforation is a medical condition characterized by the presence of a hole or opening in the nasal septum. The nasal septum is the thin wall of cartilage and bone that divides the nasal cavity into two nostrils. It plays a crucial role in maintaining the structural integrity of the nose and regulating airflow.
Nasal septum perforation, are classified according to size in three ways:
Traumatic , iatrogenic , inflammatory / malignant diseases,
infectious diseases, nasal medications and occupational causes.
Traumatic causes:
- Foreign body
- Finger injury
- Septal hematoma
- Mucosal damage
- Aggressive nose picking
- Nasal intubation
- A nasogastric tube placement
- Septoplasty (SMR ) procedure
- Rhinoplasty ( nose job ) surgery
- Wegener of granulomatous
- Churg - Strauss Syndrome
- Sarcoidosis
- Leprosy
- Leishmaniasis
- My Rhinosclero
- Squamous cell cancer
- Tuberculosis
- Syphilis
- Septal abscess
- Intranasal steroids ( intrnazal steroids)
- Vasoconstrictor drugs
- Cocaine use
- Decongestants
- Glass powder
- Mercury
- Ceramic chrome products
- Phosphorus
Cocaine using can damage the nose and cocaine cause following problems:
Cocaine causes these blood vessels which in the lining of the septum to constrict (close down). When the blood supply drops, the lining begins to die. In this case a long time causes nasal septum perforation can occur.
Prefabricated septal buttons are other therapeutic options for septal perforations. Placement of nasal septal buttons can provide improvement or resolution of epistaxis, difficulty breathing, pain, and whistling after in many of patients. There are some disadvantages of septal buttons such as, patient intolerance, local irritation, nasal obstruction and accumulation of inspissated secretions. Generally it will be removed within 6 months.
Small anterior septal perforations can be repaired with local flaps.
Sometimes, inferior turbinate flaps can be use to perforation
closure. Many of closure techniques limited to repair of nasal
septum perforations which smaller than 3 cm in diameter. Location of
perforation is not a contraindication for repairing surgery.
Generally general anesthesia can be preferred but local anestehsia
with minimal invasive techniques can be also used especially small
and anterior perforations.
Different types of connective tissue grafts can be use in the
repair of septal perforations; these included mastoid periostium,
temporalis fascia or pericranium, septal bone or cartilage, fascia
lata and acellular dermal allografts (Source:
Combining Rhinoplasty with Septal Perforation Repair).
It is difficult surgical closure of large perforations. In large perforations, some authors have suggested the use of labial and oral flaps (source: Innovative technique for large septal perforation repair and radiological evaluation). The open approach can be use to easily assesment of perforation edges and to ensure routine surgical dissection and reconstruction of the defect. Nasal hump, rib cartilages also use for repair of large septal perforation.
Dr. Heller et al. used the "Facial Artery Musculomucosal (FAMM) Flap" to repair of large nasal septal perforations. You can find detailed information at >> Repair of Large Nasal Septal Perforations Using Facial Artery Musculomucosal (FAMM) Flap
Bipedicled mucoperichondrial flaps can be used with endoscopically assisted approach in large septal pefortaions. You can find detailed information at >> Large nasal septal perforation repair by closed endoscopically assisted approach.
You can see image on the above, there is a tomography scan showed that nasal septum perforation (red arrow), right inferior turbinate (yellow arrow), left inferior turbinate (green arrow).
While different techniques exist other than thereof; surgical success is reduced while perforation diameter is increased due to decreased tissue perfusion dryer effect of the nasal airflow.
Dietary and lifestyle changes are not necessary.
Source Links >>
Repair of Nasal Septal Perforation-Surgery Overview
Surgical treatment of nasal septal perforations ...
A Review of 25-Year Experience of Nasal Septal Perforation ...
Definition of Nasal Septal Perforation
The nasal septum is a thin structure that composed from cartilage and bone. It divides the nasal cavity and it located in the middle of the nose. When the hole in the septum found, it is called as "nasal septum perforation".
Nasal septum perforation, are classified according to size in three ways:
Small holes - diameter ≤ 0.5 cm
Central holes - diameter of 0.5-2 cm
Large holes - diameter > 2 cm
Central holes - diameter of 0.5-2 cm
Large holes - diameter > 2 cm
Nasal septum perforation classification
Nasal septal perforations can vary in size, shape, and location. Healthcare professionals often use a classification system to describe and categorize nasal septal perforations based on these characteristics. While different classification systems exist, one commonly used classification is the Cottle classification. The Cottle classification categorizes nasal septal perforations based on their location within the nasal septum. Here are the different types of nasal septal perforation according to the Cottle classification:
1. Type I: Anterior Perforation
- These perforations are located in the front (anterior) part of the nasal septum.
- They are typically small in size and have a round or oval shape.
- Type I perforations are commonly associated with trauma or irritation from nasal septal surgery.
2. Type II: Posterior Perforation
- These perforations are located in the back (posterior) part of the nasal septum, closer to the nasal pharynx.
- They are typically larger in size and can have an irregular shape.
- Type II perforations can be associated with chronic nasal infections, drug abuse, or surgical complications.
3. Type III: Septal Perforation Involving the Cartilaginous and Bony Septum
- These perforations extend through both the cartilaginous and bony portions of the nasal septum.
- They can vary in size and shape and are often more challenging to repair surgically.
- Type III perforations may be associated with previous nasal surgery, trauma, or chronic inflammation.
4. Type IV: Multiple Perforations or Diffuse Perforation
- Type IV perforations involve multiple small perforations or a diffuse area of perforation throughout the nasal septum.
- They can be challenging to manage and repair surgically due to their extent and distribution.
- Type IV perforations can result from chronic inflammation, autoimmune diseases, or drug abuse.
It's important to note that while the Cottle classification provides a framework for describing nasal septal perforations, healthcare professionals may use additional criteria to assess the size, symptoms, and impact on nasal function. This helps guide treatment decisions and determine the most appropriate management approach for each individual case.
If you have a nasal septal perforation or suspect you might have one, it is recommended to consult with an otolaryngologist (ear, nose, and throat specialist) or a healthcare professional with expertise in nasal conditions. They can perform a thorough evaluation, including endoscopic examination and imaging studies if needed, to determine the classification and recommend an appropriate treatment plan tailored to your specific situation.
Causes of Perforated Nasal Septum
Nasal septal perforation causes can be classified into the
following main categories :
Causes of Nasal Perforation :
Traumatic causes:
- Finger injury
- Septal hematoma
- Mucosal damage
- Aggressive nose picking
Iatrogenic causes:
- A nasogastric tube placement
- Septoplasty (SMR ) procedure
- Rhinoplasty ( nose job ) surgery
Inflammatory / Malignant Diseases
- Churg - Strauss Syndrome
- Sarcoidosis
- Leprosy
- Leishmaniasis
- My Rhinosclero
- Squamous cell cancer
Infectious Diseases
- Syphilis
- Septal abscess
Applied Medicines in The Nose
- Vasoconstrictor drugs
- Cocaine use
- Decongestants
Occupational reasons
- Mercury
- Ceramic chrome products
- Phosphorus
Cocaine using can damage the nose and cocaine cause following problems:
- Epistaxis (nosebleed)
- Infections
- Nasal septum perforation (Cocaine Nose Hole)
- Collapse of the nose
- Loss of sense of smell
- Infections
- Nasal septum perforation (Cocaine Nose Hole)
- Collapse of the nose
- Loss of sense of smell
Cocaine causes these blood vessels which in the lining of the septum to constrict (close down). When the blood supply drops, the lining begins to die. In this case a long time causes nasal septum perforation can occur.
Cocaine damages on nose
Cocaine is a powerful stimulant drug that is commonly abused. When cocaine is used intranasally (snorted), it can cause significant damage to the nose and nasal passages. The damage is primarily due to the drug's vasoconstrictive (narrowing of blood vessels) properties and its caustic effects on the delicate nasal tissues. Here are some of the common effects and damage caused by cocaine use on the nose:
1. Nasal Septum Perforation: Prolonged and excessive cocaine use can lead to the development of a nasal septum perforation. The septum is the thin wall of cartilage and bone that separates the nostrils. The vasoconstrictive effects of cocaine reduce blood flow to the nasal tissues, leading to tissue death (necrosis) and the formation of a hole or perforation in the septum.
Cocaine-Related Nasal Septum Perforation and Intranasal Damage Video
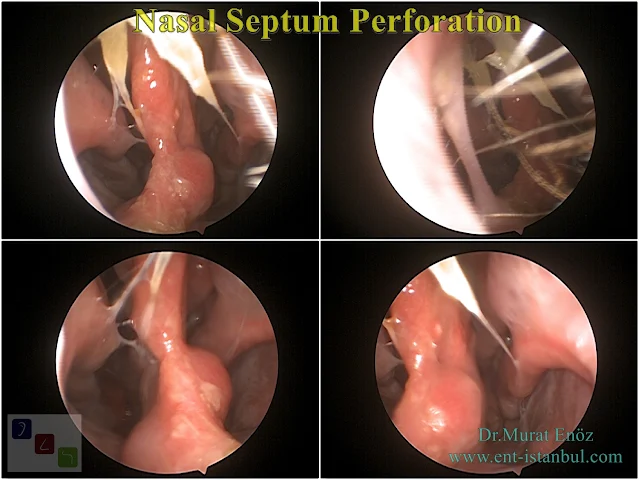
In the video above, the inside of the nose of a patient who used cocaine and had a large nasal septum defect is seen. The patient's inferior turbinates have grown towards the hole in order to slow down the rapid airflow through the perforation. However, due to the patient's continued use of cocaine, necrotic crusted mucosal damage can be seen on the anterior part of the right inferior turbinate and the inner anterior part of the left inferior tubinate due to cocaine use.
2. Nasal Ulcers and Infections: Cocaine abuse can cause the formation of nasal ulcers or sores inside the nose. These ulcers result from the drug's caustic effects on the nasal mucosa, leading to tissue damage and breakdown. The ulcers can become infected, causing nasal pain, inflammation, and recurrent infections.
3. Nasal Congestion and Rhinitis: Cocaine use can result in chronic nasal congestion, also known as "coke nose" or "coke drip." The drug's vasoconstrictive effects cause the blood vessels in the nasal passages to constrict, leading to persistent nasal stuffiness and difficulty breathing through the nose. This can also cause chronic inflammation of the nasal lining, known as rhinitis.
4. Nasal Collapse and Deformity: Prolonged cocaine use can weaken the structures supporting the nose, including the nasal cartilage and septum. Over time, this can lead to nasal collapse or deformity, causing the nose to appear misshapen or collapsed. This condition is known as "saddle nose deformity."
5. Decreased Sense of Smell: Cocaine abuse can impair the sense of smell (olfaction) due to damage to the olfactory receptors located in the nasal cavity. This can result in a diminished ability to detect and perceive odors.
6. Sinusitis and Sinus Infections: Cocaine abuse can increase the risk of developing sinusitis, which is inflammation or infection of the sinuses. The drug's caustic effects and impaired nasal function can disrupt the normal drainage of the sinuses, leading to sinus blockage and recurrent infections.
It is important to note that the damage caused by cocaine use on the nose can be irreversible in some cases. However, seeking appropriate medical care and cessation of cocaine use can help prevent further damage and manage existing symptoms. Treatment options may include medications to address symptoms, wound care for ulcers, and, in severe cases, surgical interventions to repair nasal deformities or perforations.
If you or someone you know is struggling with cocaine abuse, it is essential to seek help from healthcare professionals, addiction specialists, or support groups to address the addiction and receive appropriate treatment and support.
Cocaine side effects
Cocaine is a powerful central nervous system stimulant that can have significant side effects on both the short-term and long-term health of individuals who use it. Here are some of the common side effects associated with cocaine use:
1. Immediate effects:
- Euphoria: Cocaine use can produce intense feelings of pleasure and euphoria.
- Increased energy and alertness: Users often experience heightened energy levels, increased alertness, and a sense of being more focused.
- Dilated pupils: Cocaine can cause pupil dilation, making the pupils appear larger.
- Increased heart rate and blood pressure: Cocaine stimulates the cardiovascular system, leading to a rapid heart rate and elevated blood pressure.
- Constricted blood vessels: Cocaine causes blood vessels to constrict, which can lead to reduced blood flow and potential damage to various organs.
- Decreased appetite: Cocaine use often suppresses appetite, leading to weight loss.
2. Short-term effects:
- Agitation and restlessness: Cocaine use can induce feelings of restlessness, anxiety, irritability, and even paranoia.
- Insomnia: Stimulant properties of cocaine can interfere with sleep patterns, resulting in difficulty falling asleep or staying asleep.
- Increased body temperature: Cocaine use can cause a rise in body temperature, leading to sweating and potentially dangerous hyperthermia.
- Increased risk-taking behavior: Cocaine can impair judgment and decision-making, leading to an increased likelihood of engaging in risky behaviors, including unprotected sex or violence.
- Respiratory problems: Cocaine can irritate the respiratory system, leading to coughing, shortness of breath, or even respiratory distress.
3. Long-term effects:
- Addiction: One of the most significant risks associated with cocaine use is the development of addiction. Cocaine has a high potential for dependence, and continued use can lead to a compulsive drug-seeking behavior.
- Cardiovascular complications: Chronic cocaine use can have severe consequences on the cardiovascular system. It can lead to high blood pressure, heart palpitations, heart attacks, strokes, and other cardiovascular disorders.
- Nasal damage: Frequent snorting of cocaine can cause nasal congestion, chronic runny nose, nosebleeds, and even damage to the nasal septum, resulting in a deviated septum.
- Respiratory issues: Long-term cocaine use can lead to respiratory problems such as chronic bronchitis, lung damage, and an increased risk of respiratory infections.
- Cognitive impairment: Prolonged cocaine use may lead to cognitive deficits, including problems with attention, memory, decision-making, and impulse control.
- Psychiatric disorders: Cocaine use is associated with an increased risk of developing mental health disorders such as anxiety disorders, depression, and psychosis.
It is important to note that cocaine use can have severe and potentially life-threatening consequences. If you or someone you know is struggling with cocaine addiction or experiencing adverse side effects, it is crucial to seek professional help and support from healthcare providers or addiction treatment centers.
Septal Necrosis, Large Septal Perforation, Hard Palate Perforation, Nasal Tip and Columella Necrosis Due to Cocaine Use
In the image side , there are examination photographs of a patient who has experienced serious tissue loss due to long-term use of nasal cone. The following problems were detected in the patient:
- Very extensive septal necrosis (septum perforation)
- Columella and nasal tip necrosis
- Nasal tip collapse due to loss of nasal support tissue
- Perforation due to necrosis of the hard palate
Different large flap surgeries are required to repair the defect in both the palate and septum of the patient. In the photograph of the patient's intranasal examination, it is seen that there is serious tissue loss in the nasal cavity and the entire nasal cavity is bleeding, dry and crusty. Cocaine's circulatory deterioration caused this necrosis.
Septum Perforation Caused by Septal Piercing
In the video above, there are images during the surgery of the patient who underwent rhinoplasty surgery, and a perforation occurred in the front part of the nasal septum due to the previously used sepum piercing (warning: since this video is bloody, it may disturb the viewers, I recommend that sensitive individuals do not watch it). During the operation, this hole area is closed.
Septum piercing, a form of body modification frequently used by young people, has become widely accepted as a fashion statement in recent years. However, while the appeal of adorning the septum with jewelry is undeniable, it is important to also acknowledge the potential risks associated with this procedure. One of the most worrying complications is septum perforation, a condition that can have significant consequences for a person's health and permanent tissue damage. Septal piercing carries the risk of complications such as infection, bleeding, and allergic reactions to jewelry materials. But one of the most concerning risks is septum perforation. During the piercing process, the needle piercing the septum improperly or the jewelry putting excessive pressure on the septal tissue may cause perforation. Local infection or allergic reactions may cause the hole in the septum to enlarge and permanent epithelialization. Septum perforation, which can be caused by using a septum piercing, is a serious complication that, although rare, can have significant effects on nasal health and general health. The septum should not be punctured as full thickness as possible and the septum anatomy should be preserved. By understanding the risks, implementing appropriate aftercare, and promptly seeking medical attention for concerning symptoms, individuals can minimize the likelihood of experiencing this potentially debilitating condition.
Severe Necrosis of The Nasal Septum and Turbinates Resulting From Vasculitis
The video above shows intranasal examination images of a patient with Crohn's Disease and different vasculitic diseases. After the patient's nasal septum perforation, which started fine for 15 years, dark colored necrotic tissue pieces started to come out from the nose. As seen in the video, unfortunately, it is seen that the inside of the nose has turned into a single cavity, and there is widespread inflammatory secretion, drying and crusting.
Wegener Granulomatosis Also May Cause Nasal Septum Perforation!
Wegener's granulomatosis, also known as granulomatosis with polyangiitis (GPA), is a rare autoimmune disorder characterized by inflammation of blood vessels (vasculitis) that affects various organs, including the respiratory tract, kidneys, and other body systems. One of the common manifestations of Wegener's granulomatosis is nasal involvement, which can lead to nasal septum perforation. Here is some information about Wegener's granulomatosis and its association with nasal septum perforation:
1. Wegener's Granulomatosis: Wegener's granulomatosis is caused by an overactive immune system that mistakenly attacks healthy tissues. The exact cause of the condition is unknown, but it is believed to involve a combination of genetic and environmental factors. The immune system's abnormal response leads to inflammation and the formation of granulomas, which are clusters of inflammatory cells.
2. Nasal Involvement: Wegener's granulomatosis commonly affects the upper respiratory tract, including the nose and sinuses. Inflammation and granuloma formation in the nasal passages can cause symptoms such as nasal congestion, persistent or recurrent sinusitis, nosebleeds, and crusting. The nasal involvement in Wegener's granulomatosis can lead to complications, including nasal septum perforation.
3. Nasal Septum Perforation: Nasal septum perforation can occur in Wegener's granulomatosis due to the chronic inflammation and damage to the nasal septum. The inflammation and granuloma formation weaken the nasal septum, leading to the development of a hole or perforation. Nasal septum perforation can cause symptoms such as nasal obstruction, whistling sounds during breathing, crusting, and an increased risk of nasal infections.
4. Diagnosis and Treatment: Wegener's granulomatosis is diagnosed through a combination of clinical evaluation, blood tests, imaging studies (such as X-rays or CT scans), and sometimes a biopsy. Treatment for Wegener's granulomatosis typically involves a combination of medications to suppress the immune system and reduce inflammation. Immunosuppressive drugs, such as corticosteroids and other immunosuppressants, are commonly used to control the disease and prevent further damage.
5. Management of Nasal Septum Perforation: In cases where nasal septum perforation occurs as a complication of Wegener's granulomatosis, management focuses on controlling the underlying disease and alleviating symptoms associated with the perforation. This may involve the use of nasal saline rinses or sprays to keep the nasal passages moist, topical medications to reduce inflammation and crusting, and possibly surgical interventions to repair or close the perforation.
It is important for individuals with Wegener's granulomatosis and nasal septum perforation to receive comprehensive care from a team of healthcare professionals, including rheumatologists, otolaryngologists (ear, nose, and throat specialists), and possibly other specialists depending on the extent of organ involvement. Regular follow-up appointments and close monitoring are essential to manage the condition and minimize complications.
If you suspect you have Wegener's granulomatosis or are experiencing nasal symptoms such as nasal septum perforation, it is crucial to consult with a healthcare professional for a proper evaluation, diagnosis, and individualized treatment plan.
Symptoms of Nasal Septal Perforation
Nasal septum perforation can cause loss of laminar airflow and recirculation of air in the nasal cavity. This is associated with a symptom of nasal congestion. Large and anterior lesions are more likely to affect nasal laminar air flow and be symptomatic. A perforated septum can vary in size and location and it may be asymptomatic or cause a variety of symptoms. Small anterior septal perforations can cause a whistling noise when breathing. Larger perforations usually have more severe symptoms. These can be a combination of nasal crustation, epistaxis, difficulty breathing, nasal pressure and discomfort. The closer the perforation is to the nostrils, the more likely it is to cause symptoms.
The nasal septum, which is normally located in the midline of our nose, separates the nasal cavity into two separate air sections in a vertical oblique plane. Depending on the holes in the nasal septum, ie, due to nasal septum perforations, the air entering into the nose enters both air cavities at the same time rapidly passing through the hole in the nasal septum instead of entering two separate cavities. Due to the acceleration of the air entering the nose, it dries the mucosa, which is hit by the rapid air flow in the nose, and changes occur in the tissue over time. As seen in the photo above, it can be seen how the mucosa is dry and white in color, as the perforation of the patient with septum perforation appears to have changes in the outer nasal wall immediately adjacent to the perforation in adjacent mucosal areas.
Long-term mucosal damage due to nasal septum perforation and nasal hyperventilation
The nasal septum, which is normally located in the midline of our nose, separates the nasal cavity into two separate air sections in a vertical oblique plane. Depending on the holes in the nasal septum, ie, due to nasal septum perforations, the air entering into the nose enters both air cavities at the same time rapidly passing through the hole in the nasal septum instead of entering two separate cavities. Due to the acceleration of the air entering the nose, it dries the mucosa, which is hit by the rapid air flow in the nose, and changes occur in the tissue over time. As seen in the photo above, it can be seen how the mucosa is dry and white in color, as the perforation of the patient with septum perforation appears to have changes in the outer nasal wall immediately adjacent to the perforation in adjacent mucosal areas.
Chronic perforation of the nasal septum is associated with atrophy epithelial changes in the mucosal surface as a result of prolonged accelerated air contact. In this way, the ventilation purification and heating capacity of the nose gradually decreases over time. So, both nasal hyperventilation and mucosal changes may result in decreased nasal functions.
Diagnosis of Nasal Septal Perforation
The diagnosis of nasal septal perforation involves a comprehensive evaluation by a healthcare professional, typically an otolaryngologist (ear, nose, and throat specialist). The diagnostic process aims to determine the presence, size, location, and possible underlying causes of the nasal septal perforation. Here are the key aspects involved in the diagnosis of nasal septal perforation:
1. Medical History: The healthcare professional will begin by taking a detailed medical history, including any relevant symptoms, duration of symptoms, previous nasal surgeries or trauma, and any underlying medical conditions or medications that may contribute to nasal issues.
2. Physical Examination: A thorough physical examination of the nose and nasal passages will be conducted. The healthcare professional will visually inspect the nasal septum using a nasal speculum or an endoscope to assess for the presence of a perforation. They will also examine the surrounding nasal tissues for signs of inflammation, crusting, ulceration, or infection.
3. Nasal Endoscopy: In some cases, nasal endoscopy may be performed to obtain a more detailed view of the nasal septum and assess the extent and characteristics of the perforation. During nasal endoscopy, a thin, flexible tube with a light and camera at the tip (endoscope) is inserted into the nasal passages to visualize the nasal structures.
4. Imaging Studies: Depending on the specific situation, imaging studies such as X-rays or CT scans may be ordered to obtain a more detailed view of the nasal septum and surrounding structures. These imaging modalities can help determine the size and location of the perforation and assess the presence of any underlying abnormalities or complications.
5. Underlying Causes Evaluation: In some cases, additional tests or investigations may be needed to identify any underlying causes or contributing factors to the nasal septal perforation. Blood tests, allergy testing, or autoimmune markers may be ordered to assess for specific conditions or systemic factors that could contribute to the perforation.
6. Biopsy: In certain cases where an underlying disorder or suspicious pathology is suspected, a biopsy may be recommended. A small tissue sample from the nasal septum can be obtained for histological examination to rule out conditions such as malignancy or granulomatous diseases.
The accurate diagnosis of nasal septal perforation is essential to guide appropriate management and treatment options. Based on the findings from the diagnostic evaluation, the healthcare professional can recommend suitable treatment approaches, including conservative measures, medical interventions, or surgical repair, depending on the size, symptoms, and underlying causes of the perforation.
If you suspect you have a nasal septal perforation or are experiencing symptoms such as nasal obstruction, crusting, nosebleeds, or recurrent infections, it is important to consult with a healthcare professional, preferably an otolaryngologist, for a comprehensive evaluation and individualized treatment plan.
Nasal endoscopic examination is usually sufficient for diagnosis of septal perforation. Paranasal sinus CT scan may be required for further evaluation and differantial diagnosis.
In the photo above, nasal endoscopic appearance and sinus computed tomography of patient with septum perforation that occurring after rhinoplasty operation are showing.
Treatment of Nasal Septum Perforation
Treatment options for nasal septal perforation depend on the size and symptoms associated with the perforation. In some cases, conservative measures may be sufficient to manage symptoms, such as saline nasal rinses, nasal moisturizers, and topical medications to reduce crusting and inflammation. However, larger perforations or those causing significant symptoms may require more extensive interventions, including:
Surgical repair: This involves closing the perforation using various surgical techniques. Grafts or flaps of tissue, often taken from the nasal septum itself or other areas of the body, are used to cover the hole and promote healing.
Prosthetic devices: In cases where surgical repair is not feasible or desired, prosthetic devices such as nasal septal buttons or stents may be used to minimize symptoms and improve nasal airflow.
It is important to consult with a healthcare professional if you suspect you have a nasal septal perforation. They can evaluate your condition, provide an accurate diagnosis, and recommend appropriate treatment options based on your specific situation. Early intervention can help prevent complications and alleviate symptoms associated with nasal septal perforation.
Medical Treatment - Nasal Septal Perforation
Medical treatment for nasal septal perforation focuses on managing symptoms and promoting healing. While complete closure of the perforation may not be possible with medical interventions alone, these treatments can help alleviate symptoms and prevent further complications. It is important to consult with a healthcare professional to determine the most suitable treatment approach based on the size and symptoms associated with the nasal septal perforation. Here are some medical treatment options:
1. Nasal Saline Irrigation: Nasal saline rinses or irrigations are commonly recommended to keep the nasal passages clean and moisturized. This helps reduce crusting and dryness associated with nasal septal perforation. Saline solutions can be purchased over-the-counter or prepared at home using sterile water and salt.
2. Nasal Moisturizers: The use of nasal moisturizers or emollients can help alleviate dryness and improve comfort. These products provide a protective barrier and keep the nasal tissues hydrated. They are available in the form of nasal sprays, ointments, or gels and can be applied as directed by the healthcare provider.
3. Topical Steroids: In some cases, topical nasal steroid sprays may be prescribed to reduce inflammation and promote healing of the nasal septal perforation. These medications help alleviate symptoms such as nasal congestion, crusting, and discharge.
4. Antibiotics: If there is evidence of infection or if recurrent infections occur, the healthcare provider may prescribe antibiotics to treat or prevent bacterial infections. It is important to take antibiotics as prescribed and complete the full course of treatment.
5. Nasal Septal Buttons or Stents: Nasal septal buttons or stents are prosthetic devices that can be inserted into the nasal passage to help close the perforation temporarily and improve symptoms. These devices are typically made of silicone or other biocompatible materials. They are custom-fitted and can be worn during the day to provide support and minimize airflow through the perforation. However, they are not a permanent solution and may require regular cleaning and maintenance.
It is important to note that medical treatment alone may not fully close the nasal septal perforation. In cases where symptoms persist or the perforation causes significant discomfort, surgical intervention may be necessary. Surgical options, such as septal perforation repair using grafts or flaps, should be discussed with an otolaryngologist (ear, nose, and throat specialist) or a qualified healthcare professional with expertise in nasal conditions.
It's important to have regular follow-up appointments with the healthcare provider to monitor the progress of the nasal septal perforation and adjust the treatment plan as needed. They can provide guidance on the appropriate duration and frequency of medical treatments and evaluate if additional interventions are necessary.
Medical treatment of nasal septal perforation generally involve the topical application of agents that clean and humidify the nasal mucosa. Conjugated estrogen (Premarin), saline sprays, petroleum jelly, mixtures of various oil and petrolatum can be used.
Remember to consult with a healthcare professional for a proper evaluation and personalized treatment plan for nasal septal perforation. They can provide tailored recommendations based on your specific condition and symptoms.
Septal Button - Nasal Septal Perforation
Nasal septal buttons do not provide permanent treatment!
In patients with nasal septum perforation, it is not possible to permanently repair the existing tissue loss in the nasal septum by attaching silicone implants called septal buttons. Nazal septal buttons can be used to temporarily close the septal holes and temporarily normalize the Nazar airflow physiology in the patient. After the nasal septum perforation is closed with a septal button, nasal secretions may accumulate around the button and over time, mucosal infections may start at the edges of the perforation and the hole diameter may gradually increase. Nasal septal buttons may cause an increase in the diameter of the septum perforation in the long term and it is not appropriate to stay in the nose for years.
Surgical Repair of Nasal Septal Perforation
 |
| Surgical Repair of Nasal Septal Perforation |
There are different technique are defined to closure of nasal septum perforation. Mucosal rejuvenation techniques, crossover flap techniques, and other different flap techniques which include cartilages, mucosa with bone parts of nasal septum and adjacent tissues currently use to reparing the septal perforations. Perforation repairing surgery especially suitable for symptomatic patients.
Small anterior septal perforations can be repaired with local flaps.
 |
| In the photo above, a button-shaped cartilage graft covered by normal intranasal mucosa is seen in the perforation area of the patient who had a nasal septum perforation repair a few months ago. |
Septum Perforation Repair With Underskin Tissue and Septal Cartilage Videos and Photos:
Septal Perforation Definition, Symptoms, Treatment Video
Repair of Large Septum Perforation With Rib Cartilage Video:
Large Septum Perforation Repair With Rib Cartilage - Examination 4 Month After Surgery Video:
Before and 3 Months After Nasal Septum Perforation (4x3cm) Surgery
Nasal Septum Perforation (4x3 cm) - Before and 3 Months After Repairing Surgery Video
Open technique nasal septum perforation closure operation (using rib cartilage) was performed on the patient who applied to our clinic for the surgical treatment of a 4x3 cm septal perforation that occurred after a septorhinoplasty operation performed in another clinic. After 3 months, the patient's internal nasal silicone splints were removed and it was observed that the perforation was completely closed. This was a result that made me happy, as we knew that the perforation edges were quite dry and thin prior to the operation.
5x3.5 cm Dimensions Nasal Septum Perforation (Revision Repairing)
Very Large Nasal Septal Perforations - Surgical Difficulty
 |
| Very Large Nasal Septal Perforations - Surgical Difficulty |
It is difficult surgical closure of large perforations. In large perforations, some authors have suggested the use of labial and oral flaps (source: Innovative technique for large septal perforation repair and radiological evaluation). The open approach can be use to easily assesment of perforation edges and to ensure routine surgical dissection and reconstruction of the defect. Nasal hump, rib cartilages also use for repair of large septal perforation.
Dr. Heller et al. used the "Facial Artery Musculomucosal (FAMM) Flap" to repair of large nasal septal perforations. You can find detailed information at >> Repair of Large Nasal Septal Perforations Using Facial Artery Musculomucosal (FAMM) Flap
Bipedicled mucoperichondrial flaps can be used with endoscopically assisted approach in large septal pefortaions. You can find detailed information at >> Large nasal septal perforation repair by closed endoscopically assisted approach.
You can see image on the above, there is a tomography scan showed that nasal septum perforation (red arrow), right inferior turbinate (yellow arrow), left inferior turbinate (green arrow).
While different techniques exist other than thereof; surgical success is reduced while perforation diameter is increased due to decreased tissue perfusion dryer effect of the nasal airflow.
Postoperative Patient Care After Nasal Septal Perforation Repair
Postoperative care is crucial to ensure proper healing and minimize complications after nasal septal perforation repair surgery. Following the surgical procedure, patients will receive specific instructions from their healthcare provider. While postoperative care may vary depending on the individual case and the surgical technique used, here are some general guidelines for postoperative patient care after nasal septal perforation repair:
1. Pain Management: The healthcare provider may prescribe pain medications or recommend over-the-counter pain relievers to manage postoperative discomfort. It is important to follow the prescribed dosage instructions and take pain medication as directed.
2. Nasal Packing or Splints: In some cases, nasal packing or splints may be placed inside the nose to support the healing tissues and maintain proper alignment. These packing materials may be removed a few days (or weeks) after surgery, as instructed by the healthcare provider. Postoperatively, nasal silicone splints may stay longer than 1 week especially in patients with large perforation. Saline nasal irrigations or regular humidification is alwas useful before and after the septal perforation repairing surgery. Nasal irrigation and lubrication may provide increasing the success of the operation may improve tissue regeneration.
3. Nasal Hygiene: Proper nasal hygiene is essential for postoperative care. Patients are typically advised to perform nasal rinses or sprays using saline solution to keep the nasal passages clean and moist. The healthcare provider will provide specific instructions on the frequency and technique for nasal hygiene.
4. Avoiding Nasal Trauma: Patients should avoid activities that may cause trauma to the nose, such as vigorous nose blowing, picking the nose, or participating in contact sports. It is important to protect the nose from any accidental bumps or injuries during the healing process.
5. Medications: The healthcare provider may prescribe medications such as antibiotics or nasal sprays to prevent infection, reduce inflammation, and promote healing. It is important to take all medications as prescribed and follow the recommended treatment course.
6. Follow-up Appointments: Patients will have scheduled follow-up appointments with their healthcare provider to monitor the healing progress, remove any packing or splints if necessary, and assess the overall outcome of the surgery. It is important to attend all follow-up appointments as scheduled and communicate any concerns or changes in symptoms to the healthcare provider.
7. Lifestyle Modifications: Patients may be advised to make certain lifestyle modifications during the healing period. This may include avoiding smoking or exposure to secondhand smoke, as smoking can impair healing and increase the risk of complications.
8. Rest and Recovery: Adequate rest and proper nutrition are important for the healing process. Patients should follow any activity restrictions and give themselves enough time to recover before resuming normal activities.
It is essential to closely follow the postoperative instructions provided by the healthcare provider. If there are any concerns or unexpected symptoms, such as excessive bleeding, severe pain, or signs of infection, it is important to contact the healthcare provider immediately.
Each patient's postoperative care may vary based on individual circumstances and the specific surgical technique used. The healthcare provider will provide personalized instructions and guidance tailored to the patient's needs to ensure optimal healing and a successful recovery.
Antibiotics and pain medication are usually given for a period of first one week.
Dietary and lifestyle changes are not necessary.
Nasal Septum Perforation Repair Before and 3 Months After Video
A patient presented to our clinic after a nasal septum perforation following septorhinoplasty performed at another clinic. Upon examination, the patient was diagnosed with a 1.5 cm diameter perforation in the nasal septum, surrounded by dry, crusty mucosa, nasal septum deviation, and bone spur formation on the posterior aspect of the septum. The patient underwent open-technique septal perforation closure with temporalis fascia and cartilage grafts, septoplasty, and bone spur removal. Internal silicone splints were left in place for 3 months, and at the end of this period, the splints were removed, revealing complete closure of the perforation, correction of the septum deviation, and disappearance of the bone spur area.
Link group where you can read articles about nasal septum perforation tie published on this website >> https://www.ent-istanbul.com/search?q=Nasal+Septum+Perforation
Murat Enoz, MD, Otorhinolaryngology, Head and Neck Surgeon - ENT Doctor in Istanbul
Private Office:
Address: İncirli Cad. No:41, Kat:4 (Dilek Patisserie Building), Postal code: 34147, Bakırköy - İstanbul
Appointment Phone: +90 212 561 00 52
Appointment Phone: +90 212 561 00 52
Fax: +90 212 542 74 47




















Comments
Post a Comment