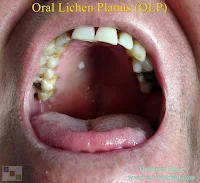
Oral Lichen Planus (OLP)
 |
| Lichen Planus in The Hard Palate and Soft Palate |
Definition of lichen planus
Lichen planus is a chronic inflammatory mucocutaneous disease. It is thought that it affects 0.5-2% of the world population. It was first described clinically by Wilson in 1869 and histologically by Dubreuilh in 1906. It is more common in women 2/3. It is more common at the beginning of the 4th and 5th decades. Oral mucosal lesions are seen in approximately half of the patients with skin lesions, but only 25% of patients have oral lesions. According to the forms of cutaneous lichen planus, oral lichen planus is a chronic disease that can persist for up to 25 years. OLP can be seen everywhere in the oral cavity, especially in the buccal mucosa, lateral parts of the tongue and gingiva are more common. It is usually observed as asymptomatic hyperkeratotic plaques or lines. Lesions may be symmetrical, bilateral or multiple in the mouth. They may be symptomatic when a secondary infection develops on asymptomatic lesions.In the photo above, in the mouth of the patient, it is seen in the hard palate and soft palate lichen planus lesions.
Lichen planus is a disease that involves skin, nail and mucosal surfaces that do not show organ involvement. They are mostly seen in the wrists, back, limbs and perimalleolar areas in adults between the ages of 30-60. Oral and genital mucous membrane lesions can also be seen. Oral lichen planus has various clinical presentations and is described as an inflammatory disease. Lichen planus is formed by T cell. Although the exact cause is not known, basal membrane or basal keratinocytes are directly affected by T lymphocytes by an immunopathological pathogenesis. Although oral lichen planus is classified among the precancerous lesions, there is little data on the prognosis of oral lichen planus-related cancers. Conversion rates between 0% and 5.6% are stated. Oral lichenoid reactions are reported to show more frequent malignant transformation than classical oral lichen planus. Local or systemic multiple therapeutic options are available for the treatment of oral lichen planus.
Etiology of lichen planus
The etiology of lichen planus is not yet known, but it is suggested that the oral mucosa may be the result of degeneration of the basal cell layer by immunological pathway. Basal cells in the OLP are the primary target for destruction. The mechanism of basal cell damage is explained by cell mediated immune reactions developed by Langerhans cells, T lymphocytes and macrophages. Langerhans cells and macrophages in the epithelial layer act as antigen servers to T cells. CD4 T cells act as helper cells and CD8 cytotoxic T cells damage the basal keratinocytes. In this process, Langerhans stimulates interleukin 1 T lymphocytes produced by cells and macrophages, and T lymphocytes proliferate by producing interleukin 2. Activated lymphocytes induce keratinocytes by producing gamma interferon and increase the differentiation by producing keratinocytes HLA DR. In this way, white lesions are formed by increasing the thickness of the surface. Modified keratinocytes are predicted as triggers of the immune response. In some cases, however, drugs or dental materials provoke this process. At the same time, viral etiology, genetic factors and lifestyle are also seen as etiological factors that may play a potential role.What are the lichen planus rashes and what symptoms do they cause?
The size of the rashes varies between 1mm and 1cm, while the border is irregular, slightly puffy, bright, red and purple causing itching. At the same time, whitish or grayish lines are observed on the debris. These stainings are grouped and have a large number. These stains on the legs and hands may also be black or brown. Lichen planus, which is not usually seen in the category of serious and dangerous diseases, may spread to the body for a long time if it is not treated. The untreated lichen planus in the mouth may increase the risk of oral cancer. Therefore, it is recommended that patients start treatment immediately and do not neglect it. The main symptom of lichen planus disease is itching.Differential diagnosis of lichen planus
Clinically, the differential diagnosis includes lichenoid reactions, leukoplakia, squamous cell carcinoma, pemphigus, mucous membrane pemphigoid and candidiasis. In Japan and Southern Europe, the prevalence of OLP was found to be high in patients with anti-HCV antibodies. It has been suggested that liver diseases disrupt the clinical course of OLP. Therefore, it is stated that liver examination should be performed in patients with OLP. Biopsy is recommended for differential diagnosis of dysplasia and malignancy in clinical diagnosis.Lichen planus and cancer risk according to its classification!
Recent studies have shown that OLP has an increased risk of developing oral cancer. This concept is generally accepted and OLP is among the precancerous lesions. The clinical classification of OLP is an important factor in follow-up. Keratotic forms, erosive, ulcerative, atrophic and plaque-like lesions; cancer development was more common in the tongue dorsum. In this respect, it is necessary to monitor the patients with OLP at least three times a year. It is important that the homogenity of the lesions is deteriorated. Oral cancer development rate is estimated to be 1-5% in patients with OLP.Lichen planus is not contagious!
Lichen planus disease, which is rarely seen, is not in the category of infectious diseases. Therefore, it is not possible to take lichen planus disease from one of them or infect someone.Treatment of oral lichen planus
Although many agents have been tried in the treatment of OLP, there is no complete treatment. Asymptomatic patients can be monitored closely without active treatment. Other medical treatments taken by the patients can be determined by changing the medication of the patient whether there is a medication about OLP. With patch tests done to patients, it can be determined whether the patient has a metal allergy. Alcohol and smoking should also be questioned. When OLP is associated with diabetes mellitus and hypertension, it is known as Grinspan syndrome and can be seen in many members of the family. But this does not indicate that OLP is a hereditary disease.Corticosteroids are considered the most useful drugs in the treatment of OLP
Because of its immunosuppressive and anti-inflammatory properties, corticosteroids are considered the most useful drugs in the treatment of OLP. Steroids can be given topically, intralesionally and systemically. In the treatment of OLP, retinoids to reduce keratinization, cyclosporin as immunosuppressants and griseofulvin as antimycotic agents are tried. Cryosurgery and CO2 laser ablation can also be applied as surgical treatment in OLP. Surgical treatment is more appropriate in plaque-like lesions.Lichen planus in the mouth is more difficult to treat than lichen planus seen in the skin
As a result of the investigations and observations, lichen planus is found in the skin of many people with lichen planus in the mouth. However, lichen planus in the mouth is more difficult to treat than lichen planus seen in the skin. Lichen planus, which directly affects cheeks, tongue and gums, lasts longer than other areas. The lichen planus, observed in the form of white dots and lines, can be easily detected. However, severe lichen planus ulcers and painful wounds may occur in the mouth. It may be necessary to determine the cause of the lichen planus in the mouth and, most importantly, take a biopsy in order to correctly diagnose it. Therefore, it is recommended that the patient should apply to the doctor as soon as possible and make the necessary examinations. Biopsy can be performed several times in order to diagnose the disease correctly.It is recommended that patients stay away from alcohol and cigarette consumption
The first step should be patient education in the treatment of the disease. As a result of the examinations and investigations, it is recommended that the cause of the lichen planus in the mouth is determined and the patient should stay away from them. The patient should be informed about the unpredictable clinic of OLP and the rationality of treatments. At the same time the patient should be warned about smoking and alcohol. Otherwise, patient dissatisfaction may be encountered. The patient's avoidance of these triggers may affect the treatment positively or prevent the increase in the severity of the disease.Source links >> Oral Lichen Planus: Symptoms, Causes & Treatment / Oral lichen planus: the clinical, historical, and therapeutic features of 100 cases / Lichen Planus - StatPearls - NCBI Bookshelf
Murat Enoz, MD, Otorhinolaryngology, Head and Neck Surgeon - ENT Doctor in Istanbul
Private Office:
Address: İncirli Cad. No:41, Kat:4 (Dilek Patisserie Building), Postal code: 34147, Bakırköy - İstanbul
Appointment Phone: +90 212 561 00 52
Appointment Phone: +90 212 561 00 52
Fax: +90 212 542 74 47


Comments
Post a Comment