About The Tonsil Removal Surgery
Tonsillectomy is a surgical procedure that involves the removal of the tonsils, which are two small masses of tissue located at the back of the throat. The procedure is typically performed to treat recurring or chronic infections of the tonsils, such as tonsillitis, or in cases where the tonsils are enlarged and causing significant breathing or swallowing difficulties.
Tonsillectomy is usually performed under general anesthesia, which means the patient is unconscious during the procedure. The surgeon uses various instruments to remove the tonsils, including a scalpel, a laser, or a specialized device that suctions and cuts the tissue. The technique used may vary depending on the surgeon's preference and the patient's specific condition.
The surgery itself usually takes about 30 minutes to an hour, and patients are typically able to return home the same day. However, in some cases, an overnight stay in the hospital may be required, especially if the patient is a child or experiences complications during the procedure.
After the surgery, it is common to experience some pain and discomfort in the throat. The patient may also have difficulty swallowing and speaking for a few days. It is important to follow the surgeon's post-operative instructions, which often include pain management strategies, such as taking prescribed pain medications, using ice packs, and consuming cold and soft foods to minimize discomfort.
Recovery time can vary from person to person, but most individuals start to feel better within a week or two. It is crucial to rest and avoid strenuous activities during the recovery period to allow the throat to heal properly. It is also important to maintain good oral hygiene, gently brushing teeth, and rinsing the mouth with saltwater or a prescribed mouthwash to reduce the risk of infection.
As with any surgical procedure, there are potential risks and complications associated with tonsillectomy. These can include bleeding during or after the surgery, infection, reactions to anesthesia, or damage to surrounding structures. It is essential to discuss these risks with the surgeon and address any concerns before undergoing the procedure.
Tonsillectomy in children is often considered when recurrent or severe tonsillitis significantly affects their quality of life. However, in recent years, there has been a shift in medical practice, and tonsillectomy is now less frequently recommended for children with milder or less frequent tonsil infections. This change is due to growing evidence suggesting that the tonsils play a role in immune function, and removing them may have long-term effects on immune system development.
In conclusion, tonsillectomy is a surgical procedure performed to remove the tonsils. It is typically recommended for individuals with recurrent or chronic tonsil infections or those experiencing significant breathing or swallowing difficulties. While the surgery can provide relief from these conditions, it is essential to carefully consider the potential risks and benefits in consultation with a qualified healthcare professional.
Does tonsillectomy operation cause autoimmune disease?
The relationship between tonsillectomy and autoimmune diseases is a topic of ongoing research and discussion. Autoimmune diseases occur when the immune system mistakenly attacks healthy cells and tissues in the body. The tonsils are part of the immune system, and their removal through tonsillectomy has led to some speculation about the potential impact on autoimmune diseases.
Some studies have suggested a potential association between tonsillectomy and an increased risk of certain autoimmune diseases. For example, research has found a possible link between tonsillectomy and an increased risk of developing autoimmune diseases such as rheumatoid arthritis, systemic lupus erythematosus, and inflammatory bowel disease. However, it is important to note that these studies have shown correlation and not necessarily causation. Further research is needed to establish a definitive cause-and-effect relationship.
It is believed that the tonsils play a role in immune system function, particularly in early life. They help in the development and maturation of the immune system by acting as a defense mechanism against pathogens. It is hypothesized that removing the tonsils may disrupt the immune system's balance, potentially contributing to an increased risk of autoimmune diseases in susceptible individuals.
However, it is essential to consider that tonsillectomy is often performed to alleviate symptoms of chronic tonsillitis or other conditions that can significantly affect an individual's quality of life. The decision to undergo tonsillectomy should be made in consultation with a healthcare professional, weighing the potential benefits against the risks.
It is important to note that the overall risk of developing autoimmune diseases after tonsillectomy appears to be relatively low, and many individuals who undergo the procedure do not experience any autoimmune-related issues. Additionally, the development of autoimmune diseases is a complex process involving multiple factors, including genetic predisposition and environmental triggers.
If you have concerns about the potential impact of tonsillectomy on autoimmune diseases, it is advisable to discuss them with a qualified healthcare professional who can provide personalized guidance based on your specific medical history and circumstances. They can provide you with the most up-to-date information and help you make an informed decision regarding your healthcare.
Tonsillectomy indications
Tonsillectomy is a surgical procedure performed to remove the tonsils, and it is typically recommended in specific situations where the tonsils are causing significant health problems. The indications for tonsillectomy can vary depending on individual circumstances, but some common indications include:
1. Recurrent or chronic tonsillitis: Tonsillitis is an infection or inflammation of the tonsils, typically caused by bacteria or viruses. If a person experiences frequent episodes of tonsillitis or has chronic tonsillitis that does not respond well to conservative treatments (such as antibiotics), tonsillectomy may be considered as a treatment option.
2. Enlarged tonsils causing breathing difficulties: Enlarged tonsils, known as tonsillar hypertrophy, can obstruct the airway and cause difficulties with breathing, especially during sleep. This condition, known as obstructive sleep apnea, can lead to daytime sleepiness, fatigue, and other health issues. Tonsillectomy may be recommended in cases where the enlarged tonsils are causing significant breathing problems.
3. Tonsil stones: Tonsil stones, also called tonsilloliths, are small, hardened deposits that form in the crevices of the tonsils. These stones can cause symptoms such as bad breath, throat discomfort, and recurrent infections. If tonsil stones are recurrent or cause significant discomfort, tonsillectomy may be considered as a treatment option.
4. Peritonsillar abscess: A peritonsillar abscess is a collection of pus that forms near the tonsils, often as a complication of untreated or severe tonsillitis. If a peritonsillar abscess is recurrent or does not respond to other treatments, tonsillectomy may be recommended to prevent further abscess formation.
5. Tonsil-related bleeding: In some cases, the tonsils may bleed spontaneously or during minor trauma, which can be a cause for concern. If an individual experiences recurrent or severe bleeding from the tonsils, tonsillectomy may be considered to alleviate the issue and prevent future bleeding episodes.
It is important to note that the decision to proceed with tonsillectomy is typically made on an individual basis, considering the patient's symptoms, medical history, and the severity of the condition. The healthcare provider will evaluate the specific circumstances and discuss the potential risks and benefits of tonsillectomy with the patient or their guardian before recommending the procedure.
In recent years, there has been a shift in medical practice, and tonsillectomy is now less frequently recommended for certain indications, such as milder or less frequent tonsillitis. This is because there is growing evidence suggesting that the tonsils play a role in immune system development and function. Therefore, healthcare providers may opt for alternative treatment options or reserve tonsillectomy for cases where it is deemed necessary.
Ultimately, the decision to proceed with tonsillectomy should be made in consultation with a qualified healthcare professional who can assess the individual situation and provide personalized recommendations based on the best available evidence and medical guidelines.
Tonsillectomy contrendications
Tonsillectomy, like any surgical procedure, has certain contraindications or situations where the surgery may not be recommended. These contraindications are typically determined by the surgeon and healthcare team based on individual patient factors and medical history. Some common contraindications for tonsillectomy include:
1. Bleeding disorders: Individuals with bleeding disorders, such as hemophilia or von Willebrand disease, may be at an increased risk of excessive bleeding during and after surgery. Tonsillectomy may be contraindicated in such cases due to the potential for complications.
2. Current infection: If a patient has an active infection, such as severe tonsillitis or an abscess, it is generally recommended to delay the tonsillectomy until the infection has resolved. Performing surgery during an active infection can increase the risk of complications and hinder the healing process.
3. Uncontrolled medical conditions: Tonsillectomy may be contraindicated in individuals with uncontrolled or poorly managed medical conditions, such as diabetes, hypertension, or heart disease. These conditions can increase the risk of complications during and after surgery.
4. Immunodeficiency: Patients with compromised immune systems, either due to an underlying medical condition or medication use, may have an increased risk of infection and slower wound healing. Tonsillectomy may be contraindicated or require special precautions in such cases.
5. Previous radiation therapy: Individuals who have undergone radiation therapy in the head and neck region may have compromised tissue healing and increased risk of complications. Tonsillectomy may be contraindicated or require additional evaluation and planning in these situations.
6. Severe obesity: Obesity can be associated with an increased risk of surgical complications, such as difficulties with anesthesia, breathing, and wound healing. Tonsillectomy in severely obese individuals may require careful evaluation and consideration of the potential risks and benefits.
7. Age considerations: Tonsillectomy is generally considered safe for both children and adults. However, there may be specific considerations for very young children or older adults, such as evaluating their ability to tolerate anesthesia and surgery. Age-related factors may influence the decision to proceed with tonsillectomy.
It is important to note that contraindications may vary depending on the specific circumstances and the surgeon's judgment. The decision to proceed with tonsillectomy or consider alternative treatment options should be made in consultation with a qualified healthcare professional who can evaluate individual factors and provide personalized recommendations.
Best tonsillectomy technique
There is no universally recognized "best" tonsillectomy technique, as the choice of technique can vary depending on several factors, including the patient's age, medical history, surgeon's expertise, and the specific indications for tonsillectomy. However, I can provide an overview of some commonly used techniques:
1. Cold knife/Steel dissection: This technique involves using a scalpel or scissors to dissect and remove the tonsils. It is a traditional method that has been used for many years. The surgeon carefully separates the tonsil tissue from the surrounding structures before excising them. This technique allows for precise removal of the tonsils but may involve a longer operative time and potentially more postoperative pain.
2. Electrocautery: In this technique, an electrocautery device is used to cut and remove the tonsils. The device applies heat and electrical current to simultaneously cut and seal blood vessels, reducing the risk of bleeding during the procedure. Electrocautery can help reduce operative time but may result in more postoperative pain compared to other techniques.
3. Harmonic scalpel: The harmonic scalpel utilizes ultrasonic energy to cut and coagulate tissue during tonsillectomy. It provides a combination of cutting and cauterizing effects, allowing for more precise dissection and potentially reducing the risk of bleeding. The use of the harmonic scalpel may result in less postoperative pain and faster recovery compared to other techniques.
4. Coblation: Coblation uses radiofrequency energy to remove the tonsils. The technique involves ionizing saline solution into plasma, which dissolves and removes the tonsil tissue. Coblation provides precise tissue removal while minimizing damage to surrounding structures and reducing the risk of bleeding. This technique has been associated with reduced postoperative pain and faster recovery for some patients.
5. Laser tonsillectomy: Laser-assisted tonsillectomy involves using a laser beam to remove the tonsils. The laser energy vaporizes and seals blood vessels, reducing bleeding during the procedure. Laser tonsillectomy can provide precise tissue removal, but it may be associated with a longer operative time and potentially higher cost.
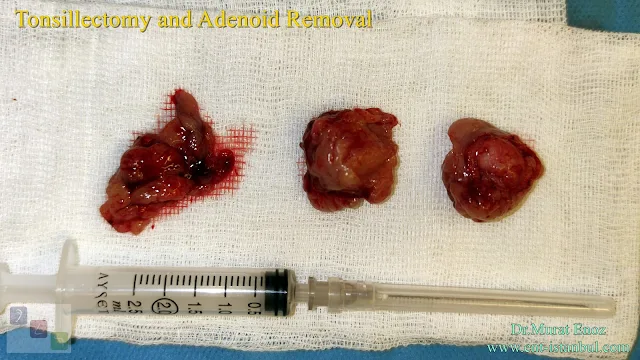
6. Thermal welding device: During the tonsillectomy operation performed with this device, the heat damage to the adjacent tissue is considerably reduced. Recovery time after the procedure is very fast. In the photo above, a bilateral tonsillectomy operation was performed using a thermal welding device. The device has two different modes. The first mode is the coagulation mode, in which bleeding areas are settled. The mode of the twin is cutting mode and tissue cutting is done in this mode. If the coagulation mode is used sparingly, heat damage is greatly reduced. As seen in the photo above, post-procedure anterior and posterior folds were sutured with 4/0 vicryl.
It is important to note that the choice of technique should be based on a thorough evaluation of the patient's condition and individual factors, as well as the surgeon's expertise and preference. The surgeon will consider factors such as the severity of the tonsil condition, risk of bleeding, postoperative pain management, and potential benefits and risks associated with each technique.
Ultimately, the goal of any tonsillectomy technique is to safely and effectively remove the tonsils while minimizing complications and promoting a smooth recovery. It is essential to have a detailed discussion with a qualified healthcare professional to determine the most appropriate technique for an individual's specific needs.
Tonsillectomy versus Tonsillotomy
Tonsillectomy and tonsillotomy are two surgical procedures performed to address issues related to the tonsils, which are part of the lymphatic system located at the back of the throat. While both procedures involve the removal of the tonsils, they differ in terms of the extent of tissue removal and the conditions they are commonly used to treat. Let's explore the differences between tonsillectomy and tonsillotomy.
1. Tonsillectomy:
Tonsillectomy is a surgical procedure that involves the complete removal of the tonsils. It is typically performed under general anesthesia and is considered a more extensive procedure. Tonsillectomy is often recommended in the following situations:
a. Recurrent Tonsillitis: When a person experiences frequent episodes of tonsillitis (inflammation of the tonsils) that do not respond well to non-surgical treatments, such as antibiotics, a tonsillectomy may be considered.
b. Enlarged Tonsils: Tonsils that are excessively large and causing problems with breathing, swallowing, or sleeping may be removed through a tonsillectomy.
c. Tonsil-related Sleep Disorders: In some cases, enlarged tonsils can obstruct the airway during sleep, leading to conditions like sleep apnea. Tonsillectomy can help alleviate the obstruction and improve breathing during sleep.
2. Tonsillotomy:
Tonsillotomy, also known as partial tonsillectomy or intracapsular tonsillectomy, is a less invasive surgical procedure compared to tonsillectomy. Instead of completely removing the tonsils, tonsillotomy involves removing only a portion of the tonsillar tissue. It is usually performed under general anesthesia or local anesthesia with sedation. Tonsillotomy is commonly recommended in the following scenarios:
a. Obstructive Sleep Apnea (OSA): Tonsillotomy may be considered as a treatment option for children with obstructive sleep apnea who have enlarged tonsils. By removing part of the tonsillar tissue, the obstruction can be reduced, improving breathing during sleep.
b. Milder Tonsillitis: If a person experiences less severe and infrequent episodes of tonsillitis, tonsillotomy may be preferred over tonsillectomy. It can help reduce the frequency and severity of tonsillitis while preserving a portion of the tonsils.
c. Faster Recovery: Compared to tonsillectomy, tonsillotomy generally involves a faster recovery period, as the procedure is less extensive and causes less post-operative pain.
It's important to note that the choice between tonsillectomy and tonsillotomy depends on various factors, including the severity of the condition, individual patient characteristics, and the recommendation of a healthcare professional.
Both tonsillectomy and tonsillotomy are generally safe procedures; however, as with any surgical intervention, there are potential risks and complications that should be discussed with a healthcare provider before making a decision.
Overall, while tonsillectomy involves the complete removal of the tonsils and is typically performed for more severe cases, tonsillotomy is a partial removal option that can be considered for milder conditions, aiming to achieve similar benefits with a less invasive approach.
Bleeding After Tonsillectomy Operation
Bleeding after a tonsillectomy is a potential complication that can occur in some cases. Postoperative bleeding is one of the main concerns following this surgical procedure. While it is relatively uncommon, it is important to be aware of the signs, risks, and management of bleeding after a tonsillectomy.
1. Types of bleeding:
There are two main types of bleeding that can occur after a tonsillectomy:
a. Primary bleeding: This type of bleeding occurs within the first 24 hours after the surgery. It is often related to surgical techniques, such as inadequate control of blood vessels during the procedure or the dislodgment of a blood clot that has formed.
b. Secondary bleeding: Secondary bleeding occurs after the initial 24-hour period following the tonsillectomy. It is usually associated with the scab formation and subsequent detachment from the surgical site. Secondary bleeding can happen up to 10-14 days after the procedure.
2. Signs and symptoms:
Signs of bleeding after a tonsillectomy may include:
- Frequent swallowing or spitting up blood.
- Bleeding from the nose, mouth, or throat.
- Gagging or vomiting blood.
- Blood in saliva or phlegm.
- Feeling faint, dizzy, or lightheaded.
- Increased heart rate.
- Pallor (pale appearance).
- Persistent or worsening pain.
If you experience any of these symptoms, it is crucial to seek immediate medical attention.
3. Risks and factors:
Several factors can increase the risk of bleeding after a tonsillectomy, including:
- Age: Children, especially those under 3 years old, are at higher risk.
- Genetics: Certain individuals may have a genetic predisposition to bleeding.
- Medications: Blood-thinning medications, such as aspirin or nonsteroidal anti-inflammatory drugs (NSAIDs), can increase the risk.
- Inadequate rest or activity: Strenuous activities that can strain the surgical site should be avoided.
- Poor postoperative care: Not adhering to postoperative instructions, such as avoiding hard or sharp foods, can increase the risk of bleeding.
4. Management:
If bleeding occurs after a tonsillectomy, immediate medical attention is crucial. Depending on the severity of the bleeding, the management may involve:
- Observation: In cases of mild bleeding, close monitoring may be sufficient, and the bleeding may stop on its own.
- Intervention: If the bleeding is persistent or significant, medical intervention may be necessary. This can involve several methods, such as cauterization (sealing the bleeding blood vessels) or applying pressure to the bleeding site.
- Blood transfusion: In severe cases of bleeding, a blood transfusion may be required to replace the lost blood volume.
It's important to follow the postoperative care instructions provided by your healthcare team to minimize the risk of bleeding. This typically includes avoiding strenuous activities, taking prescribed pain medications, maintaining good oral hygiene, and consuming a soft diet.
Remember, while bleeding after a tonsillectomy can be concerning, it is relatively rare. Most patients recover without complications. However, if you experience any signs of bleeding, promptly reach out to your healthcare provider for appropriate evaluation and management.
Health Benefits of Tonsillectomy Operation
Tonsillectomy, the surgical removal of the tonsils, can have several positive effects on a person's health. These include:
1. Reduction in Tonsillitis: Tonsillectomy can significantly reduce the frequency and severity of tonsillitis, a condition characterized by recurrent inflammation and infection of the tonsils. By removing the tonsils, the source of infection is eliminated, leading to a decrease in throat infections.
2. Improved Breathing: Enlarged tonsils can obstruct the airway and cause difficulties in breathing, especially during sleep. Tonsillectomy can alleviate this obstruction, improving airflow and breathing patterns, which can enhance overall respiratory function.
3. Alleviation of Sleep-Related Disorders: Enlarged tonsils are often associated with sleep-related disorders such as sleep apnea, where breathing is interrupted during sleep. By removing the tonsils, airway obstruction is reduced, leading to improved sleep quality and decreased symptoms of sleep apnea.
4. Reduced Antibiotic Use: Chronic tonsillitis often requires frequent antibiotic treatment to manage infections. Tonsillectomy can decrease the need for long-term antibiotic use, minimizing the risks associated with antibiotic resistance and potential side effects of medications.
5. Enhanced Quality of Life: By reducing the frequency of throat infections, improving breathing, and alleviating sleep-related issues, tonsillectomy can contribute to an overall improvement in the quality of life. It can lead to fewer missed school or work days, improved energy levels, and better overall health.
It's important to note that the decision to undergo a tonsillectomy should be made in consultation with a healthcare professional. They will evaluate the individual's specific condition and determine whether the potential benefits outweigh the risks associated with the surgery.
Recovery After Tonsillectomy Operation
Recovery after a tonsillectomy operation typically involves a period of healing and adjustment. Here are some key aspects of the recovery process:
1. Immediate Postoperative Period: After the surgery, patients are usually monitored in a recovery area until they are awake and their vital signs are stable. It's common to experience a sore throat, mild to moderate pain, and possibly nausea or vomiting due to the anesthesia. Pain medications and anti-nausea medications may be prescribed to manage these symptoms.
2. Hospital Stay or Outpatient Procedure: Depending on the individual case, tonsillectomy can be performed as an outpatient procedure, allowing patients to return home on the same day, or require a short hospital stay for monitoring. The healthcare team will provide instructions for postoperative care and discharge.
3. Pain Management: Pain and discomfort are common during the recovery period. Over-the-counter pain relievers, such as acetaminophen or ibuprofen, are often recommended. Stronger prescription pain medications may be prescribed for severe pain, but they should be used as directed. It's essential to follow the healthcare provider's recommendations for pain management.
4. Diet and Fluid Intake: Initially, a soft or liquid diet is advised to avoid irritating the surgical site. Cold or lukewarm liquids and foods are often recommended to help soothe the throat. It's crucial to stay hydrated by drinking plenty of fluids, but avoid using straws, as they can increase the risk of bleeding.
5. Rest and Recovery Time: Adequate rest and recovery are vital during the healing process. It's important to plan for time off work or school to allow the body to heal. Avoiding strenuous activities, including heavy lifting or exercise, is typically advised for about two weeks or as recommended by the healthcare provider.
6. Follow-Up Appointments: Follow-up appointments with the healthcare provider are usually scheduled to monitor the healing progress, manage any potential complications, and remove any dissolvable stitches if needed. It's important to attend these appointments and communicate any concerns or unusual symptoms experienced during the recovery period.
7. Gradual Return to Normal Activities: As the healing progresses, gradually reintroduce normal activities based on the healthcare provider's recommendations. This includes resuming regular diet, physical activities, and returning to work or school. However, it's crucial to listen to the body and avoid overexertion or pushing too quickly.
Recovery time can vary from person to person, but it typically takes about one to two weeks to return to normal activities. It's important to follow the postoperative care instructions provided by the healthcare team and reach out to them if there are any concerns or unexpected symptoms during the recovery process.
Tonsillectomy Operation in Older Patients
Tonsillectomy, the surgical removal of the tonsils, can be performed in older patients as well, although it may present some unique considerations compared to younger individuals. Here are some key points regarding tonsillectomy in older patients:
1. Age-related Factors: Older patients may have certain age-related factors that need to be taken into account. These include the presence of underlying health conditions, reduced immune function, and potential challenges in the healing process. It's essential for the healthcare provider to assess the overall health of the patient and determine the suitability of the procedure.
2. Increased Risk of Complications: Older patients may have a higher risk of complications during and after surgery compared to younger individuals. This can include a higher risk of bleeding, infections, or adverse reactions to anesthesia. The healthcare team will carefully evaluate the patient's medical history, perform preoperative assessments, and take appropriate precautions to minimize these risks.
3. Benefits for Older Patients: Despite the potential risks, tonsillectomy in older patients can offer various benefits. Removal of infected or enlarged tonsils can alleviate chronic tonsillitis, improve breathing and airflow, reduce sleep-related disorders, and enhance overall quality of life. These benefits should be carefully weighed against the potential risks and individual patient factors.
4. Preoperative Assessment: Older patients undergoing tonsillectomy will typically undergo a comprehensive preoperative assessment. This may include blood tests, imaging studies, and consultation with specialists to ensure their suitability for surgery. The healthcare provider will review the patient's medications and medical history to manage any potential risks or interactions.
5. Postoperative Care: Recovery after tonsillectomy in older patients may require additional attention and monitoring. Pain management and postoperative instructions regarding diet, hydration, and activity restrictions are crucial. Older patients may experience longer recovery times and may need more support during the healing process. Adequate rest, pain control, and close communication with the healthcare team are essential for optimal recovery.
6. Individualized Approach: The decision to proceed with tonsillectomy in older patients is made on an individual basis, considering the patient's overall health, severity of symptoms, and expected benefits. The healthcare provider will discuss the potential risks, benefits, and alternatives with the patient and involve them in the decision-making process.
It's important for older patients considering tonsillectomy to have a thorough discussion with their healthcare provider to understand the procedure, potential risks, and expected outcomes. The healthcare team will provide personalized care and guidance to ensure a safe and successful surgery.
Is There an Age Limit for Tonsillectomy Operation?
The decision to perform a tonsillectomy is typically based on an individual's specific medical condition rather than a strict age limit. While tonsillectomy is commonly associated with children, it can be performed in individuals of various age groups, including adults and older patients. However, there are certain considerations when determining the appropriateness of tonsillectomy based on age:
1. Children: Tonsillectomy is relatively common in children, especially if they experience recurrent or severe tonsillitis, sleep-disordered breathing, or other tonsil-related complications. Generally, the decision to proceed with tonsillectomy in children is based on the frequency and severity of symptoms and the impact on the child's quality of life. While it is written in old sources that tonsillectomy operation may be inconvenient under the age of 3; In new sources, it is written that tonsillectomy operation can be performed from 16 months of age. Although there is no specific age limit for this, infants and children with advanced tonsillar hypertrophy may have post-procedure oxygen rush and lower respiratory tract edema. It is appropriate for small babies to be operated in fully equipped hospitals.
2. Adults: Tonsillectomy in adults is less common but may be recommended in cases of recurrent or chronic tonsillitis, enlarged tonsils causing breathing difficulties, or sleep-related issues. The decision is typically made based on the individual's symptoms, overall health, and the potential benefits of the surgery.
3. Older Adults: Tonsillectomy can be performed in older adults as well, but age-related factors such as overall health, comorbidities, and potential surgical risks need to be carefully considered. The decision is made on an individual basis, taking into account the specific circumstances and the potential benefits of the procedure.
It's important to note that there is no specific age limit for tonsillectomy. The suitability for the procedure is determined by evaluating the individual's symptoms, medical history, and the potential benefits versus the risks associated with the surgery. The healthcare provider will assess the specific condition and make a recommendation based on the individual's unique circumstances.
Ultimately, the decision to proceed with tonsillectomy should be made in consultation with a healthcare professional who can provide personalized guidance and weigh the potential benefits and risks for the individual patient.
Link group where you can read the articles I prepared about tonsillectomy operation on this website >> https://www.ent-istanbul.com/search?q=tonsillectomy+operation
Source links >>
- Awareness and Perceptions of the Impact of Tonsillectomy on the Level of Immunity and Autoimmune Diseases among the Adult Population in Abha City, Kingdom of Saudi Arabia - PMC (nih.gov)
- Coblation versus other surgical techniques for tonsillectomy - PMC (nih.gov)
- Systematic review of analgesics and dexamethasone for post-tonsillectomy pain in adults - PMC (nih.gov)
Murat Enoz, MD, Otorhinolaryngology, Head and Neck Surgeon
Private Office:
Address: İncirli Cad. No:41, Kat:4 (Dilek Patisserie Building), Postal code: 34147, Bakırköy - İstanbul
Appointment Phone: +90 212 561 00 52
Appointment Phone: +90 212 561 00 52
Fax: +90 212 542 74 47





.jpg)

Comments
Post a Comment